- About
- Blog
- Infertility
- IVF Treatments
- New IVF Advances
- Mitochondrial Replacement Therapy!
- IVF Treatment in Cyprus
- IUI
- Mini IVF
- IVF + ICSI
- Cytoplasmic IVF
- Tandem IVF Cycle
- Egg Donation
- Embryo Donation
- Sperm Donation
- Gender – Sex Selection
- Gestational Surrogacy
- Same Sex Gay Surrogacy
- Surgical Sperm Retrieval
- Pre Implantation Genetic Diagnosis PGD
- Egg Freezing
- Gender Selection Using Donor Eggs
- Sickle Cell Disease Prevention
- F.A.Q.
- Travel
- About
- Blog
- Infertility
- IVF Treatments
- New IVF Advances
- Mitochondrial Replacement Therapy!
- IVF Treatment in Cyprus
- IUI
- Mini IVF
- IVF + ICSI
- Cytoplasmic IVF
- Tandem IVF Cycle
- Egg Donation
- Embryo Donation
- Sperm Donation
- Gender – Sex Selection
- Gestational Surrogacy
- Same Sex Gay Surrogacy
- Surgical Sperm Retrieval
- Pre Implantation Genetic Diagnosis PGD
- Egg Freezing
- Gender Selection Using Donor Eggs
- Sickle Cell Disease Prevention
- F.A.Q.
- Travel
Mitochondrial Replacement Therapy
A Groundbreaking New Medical Technique
Dr. Shoukhrat Mitalipov, a world-renowned medical geneticist, who is mostly known for his ground-breaking work on mitochondrial replacement therapy, is now merging forces with North Cyprus IVF Center at Elite Hospital. Dr. Mitalipov has been the recipient of many accolades for his ground-breaking work on genetics and stem cell research.
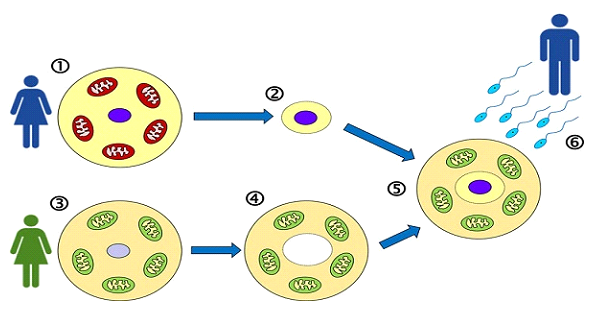
Developed by Dr. Shoukhrat Mitalipov, Mitochondrial replacement therapy (MRT) is a groundbreaking medical technique that involves replacing faulty mitochondria in an egg to prevent the transmission of mitochondrial diseases from a mother to her offspring. It can also be used in women with oocyte aging where aging mitochondria and cytoplasmic organelles do not provide a suitable environment for fertilization to occur.
Mitochondria are the energy-producing organelles in cells. Mitochondria control respiration and energy production within every cell of the body, so when the mitochondria age or they lessen in number, the drive for cellular energy production and other cellular processes downstream are directly impaired.
MRT is different from cytoplasmic transfer. In cytoplasmic transfer, a portion of a woman’s eggs cytoplasm is replaced with a portion of an egg donor’s cytoplasm. It isn’t possible to visualize the mitochondria when the transfer is performed, whereas with MRT, you have visualization. So, with cytoplasmic transfer, you have more mitochondria than with your own oocytes, which assists and increases mature age success rates by 5%. MRT, on the other hand, is performed via a method called Maternal Spindle Transfer. In this method, the nucleus from a mother’s egg is transferred into a donor egg that has had its own nucleus removed but retains healthy mitochondria. The reconstructed egg is then fertilized with sperm. With MRT, you have the full young oocyte number of mitochondria.
This technique aims to create embryos free of harmful mitochondrial mutations, thus reducing the risk of mitochondrial diseases. It further allows women in advanced age brackets to conceive their own biological children as their own genetic material is provided with a healthy host environment which makes cell division, growth, and development possible.
One of the most notable clinical trials involving mitochondrial replacement therapy took place in Greece, under the guidance of Dr. Mitalipov. This trial was significant because it marked one of the first attempts to apply MRT in a clinical setting to address issues of infertility believed to be linked to poor egg quality possibly due to bad mitochondrial health.
In April 2019, this trial led to the birth of a healthy baby boy in Greece using the maternal spindle transfer technique. The procedure was part of a clinical research project aimed at women who had failed multiple IVF attempts due to poor egg quality. The success of this birth demonstrated the potential of MRT not only to prevent mitochondrial disease but also to assist in overcoming infertility problems associated with mitochondrial dysfunction in eggs. During this trial, success rate was quoted at 25%.
Now, with joined forces of Dr. Mitalipov’s team and Dr. Ozyigit’s team, MRT has become a treatment option for women in advanced age brackets. This treatment is not being run as a clinical trial. It has now been incorporated into IVF treatments offered at North Cyprus IVF Center.
MRT will require multiple egg retrievals for most women. In most IVF treatments where the female patient is over the age of 40, oocyte count and quality become a concern. While MRT aims to correct the latter, the former is an issue that cannot be addressed with MRT alone. Patients in older age brackets who do not produce sufficient number of oocytes in a single controlled ovarian hyperstimulation protocol, two or sometimes three egg collections may be necessary in order to obtain multiple oocytes that can be used in an IVF cycle with the advanced method of MRT.
If multiple egg collection is necessary, egg(s) obtained after each cycle will be frozen. Once a sufficient number of oocytes has been achieved, all oocytes are then thawed where they undergo MRT treatment with freshly obtained donor oocytes. Donor oocytes are always obtained fresh for the purposes of MRT treatment as the mitochondria and the rest of the cytoplasmic organelles need to be in their most viable shape. Once fertilization takes place via ICSI, the embryos are incubated for further development. Once the embryos reach the blastocyst stage, they are frozen to be transferred at a later date.
In order to receive the embryo(s), the female patient receives treatment for endometrial preparation as part of her frozen embryo transfer.
The cost of this treatment modality depends on the mumber of oocyte retrievals to be performed. However, on average, each patient is expected to undergo two oocyte retrievals, resulting in an expected cost of 14,000 Euros for the entire treatment from the beginning to the end. This total cost includes two rounds of egg collection, freezing, MRT treatment and a subsequent embryo transfer.
Who is an ideal candidate for mitochondrial replacement therapy?
This treatment modailty is primarily recommended for wome who have documented mitochondrial dysfunction, those in older age brackets with diminished mitochondrial function, and women who have experienced multiple unsuccessful IVF cycles using their own oocytes, which may be attributed to mitochondrial aging and dysfunction.
What is the success rate of IVF treatment with mitochondrial replacement therapy?
While this is a question that can have different answers depending on the indication for MRT, in women who have previously undergone multiple failed IVF cycles due to oocyte aging or oocyte quality concerns, the success of MRT procedure has been found to be 25%, meaning 1 in 4 women became pregnant undergoing an IVF cycle with mitochondrial replacement therapy. This is a significant number considering these patients already had multiple failed IVF cycles with their own oocytes and were not being considered for further IVF cycles with own oocytes.
How long should I stay in Cyprus for this treatment?
Majority of our patients come from abroad for various fertility treatments. For our patients with a busier schedule, the preliminary work of testing and medication usage can be organized in a remote fashion. This would involve having labs done locally and sharing the results with us. With your laboratory work and scan results, we can design a treatment protocol and send you the relevant prescription. During the initial preparatory period, you will be able to use your medication and have your scans at home. You will be required to fly to Cyprus for your trigger injection and the oocyte retrieval procedure. We estimate this period to be a minimum of 3 and maximum of 5 days. This would be the same for each oocyte retrieval cycle.
Once MRT has been performed and your embryos have been created, you will have a final treatment for making your endometrium receptive of the embryo(s) to be transferred. On this occasion, you will be required to come to Cyprus for a total of 2 days.
North Cyprus IVF Centre
North Cyprus IVF Centre is a patient focused fertility clinic, located within “Elite Research and Surgical Hospital” in Nicosia, Cyprus. Our clinic is one of the most advanced fertility clinics in the world, offering a wider selection of treatment options at affordable prices.
Contact Us
Phone
English: +90 548 875 8000
French: +90 548 876 8000
Turkish: +90 542 869 8000
Arabic: +90 548 875 8000
German: +90 548 830 1987
Russian: +90 548 828 9955
info@northcyprusivf.net
© 2020 LowCostIVF - All rights reserved. Privacy Policy