- About
- Blog
- Infertility
- IVF Treatments
- New IVF Advances
- Mitochondrial Replacement Therapy!
- IVF Treatment in Cyprus
- IUI
- Mini IVF
- IVF + ICSI
- Cytoplasmic IVF
- Tandem IVF Cycle
- Egg Donation
- Embryo Donation
- Sperm Donation
- Gender – Sex Selection
- Gestational Surrogacy
- Same Sex Gay Surrogacy
- Surgical Sperm Retrieval
- Pre Implantation Genetic Diagnosis PGD
- Egg Freezing
- Gender Selection Using Donor Eggs
- Sickle Cell Disease Prevention
- F.A.Q.
- Travel
- About
- Blog
- Infertility
- IVF Treatments
- New IVF Advances
- Mitochondrial Replacement Therapy!
- IVF Treatment in Cyprus
- IUI
- Mini IVF
- IVF + ICSI
- Cytoplasmic IVF
- Tandem IVF Cycle
- Egg Donation
- Embryo Donation
- Sperm Donation
- Gender – Sex Selection
- Gestational Surrogacy
- Same Sex Gay Surrogacy
- Surgical Sperm Retrieval
- Pre Implantation Genetic Diagnosis PGD
- Egg Freezing
- Gender Selection Using Donor Eggs
- Sickle Cell Disease Prevention
- F.A.Q.
- Travel
Preimplantation Genetic Testing in IVF Cycles
Overview of Pre-Implantation Genetic Testing
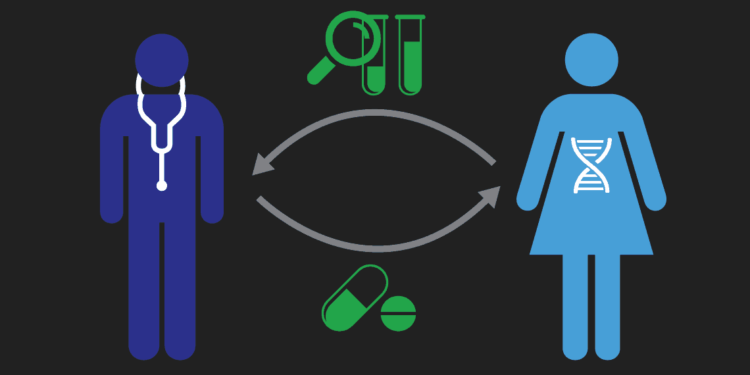
Pre-Implantation Genetic Testing is a new generation embryo testing method which offers both an alternative to prenatal genetic testing methods such as chorionic villus sampling (CVS) and amniocentesis for couples who are known to have a high risk of transmitting a genetic disorder to their offspring as well as a testing platform for patients with recurrent IVF failures and recurrent miscarriages.
While prenatal genetic testing methods can be employed only at a certain time during pregnancy, PGT offers genetic testing on embryos prior to pregnancy, therefore, eliminating the likelihood of being pregnant with an offspring with genetic problems. The origins of PGD/PGS dates back to 1968 when Edwards and Gardner performed the very first micro-surgical embryo biopsy on rabbit embryos by staining rabbit blastocyst sex chromatin with euchrysine 2GNX. However, it was not until the early 1990s where the first PGT case was performed to screen sex of the embryo for a sex-linked autosomal recessive disorder.
Preimplantation genetic testing (PGT) is a critical advancement in assisted reproductive technology (ART), specifically in in vitro fertilization (IVF). PGT involves genetic analysis of embryos before uterine transfer, aiming to enhance implantation rates, reduce miscarriage risks, and prevent the transmission of genetic disorders. The technology has evolved significantly over the past few decades and is categorized into three main types: PGT-A (for aneuploidy screening), PGT-M (for monogenic or single-gene disorders), and PGT-SR (for structural rearrangements). Below, you will find information on different types of PGT, the clinical scenarios they are suited for, and their overall efficacy.
Types of Preimplantation Genetic Testing
1. PGT-A (Preimplantation Genetic Testing for Aneuploidy)
PGT-A screens embryos for numerical chromosomal abnormalities (aneuploidy). Aneuploidies are a leading cause of implantation failure, miscarriage, and chromosomal disorders like Down syndrome (trisomy 21), Patau syndrome (trisomy 13) and Edwards syndrome (trisomy 18).
Indications:
Advanced maternal age (>35 years), where aneuploidy rates increase due to age-related chromosomal segregation errors.
Recurrent implantation failure or repeated IVF failures.
Recurrent pregnancy loss (RPL), often associated with chromosomal abnormalities in embryos.
Male factor infertility, as aneuploidy risk can increase with certain sperm abnormalities.
Gender selection for family balancing purposes
Procedure:
Embryos are biopsied (usually at the blastocyst stage) to extract a few trophectoderm cells, which are then analyzed using techniques such as FISH or next-generation sequencing (NGS), depending on the purpose of treatment. In cases where gender selection is the primary focus with no background of genetic diseases, a simple FISH analysis can provide a basic 5-chromosome panel that tests for the most common genetic disorders on chromosomes 13, 18 and 21 as well as X and Y.
Success and Limitations:
PGT-A has been shown to improve live birth rates in certain populations, such as older women and those with prior failed cycles, but its universal application remains controversial. Some studies suggest no significant benefit in younger patients with good prognosis (Munné et al., 2019). Moreover, mosaicism—where some cells in the embryo are normal, and others are aneuploid—can complicate interpretation and outcomes. In many cases, embryos that have been deeme mosaic can go on to eliminate mosaicism and develop into genetically healthy and euploid embryos. When PGT-A is performed in young and healthy populations, this can cause discarding of embryos that can potentially develop into genetically healthy human beings. Overall, this is a suitable option for patients opting for gender selection for family balancing purposes, patients with repeated IVF failures or recurrent miscarriages.
2. PGT-M (Preimplantation Genetic Testing for Monogenic Disorders)
PGT-M identifies embryos carrying single-gene disorders (e.g., cystic fibrosis, sickle cell anemia, Huntington’s disease). Couples who are carriers of a known genetic mutation or have a family history of a specific genetic condition benefit from this testing.
Indications:
– Carrier screening for autosomal recessive or dominant conditions.
– Prevention of X-linked disorders (e.g., Duchenne muscular dystrophy, hemophilia).
– Couples with a known pathogenic variant in one or both partners.
Procedure:
This involves customized testing using techniques like polymerase chain reaction (PCR) or NGS to detect the specific mutation. Often, linkage analysis is performed alongside mutation detection to confirm results and reduce the risk of misdiagnosis. This means, the couple seeking testing with PGT-M will need to have a detailed genetic testing showing the specific gene mutations so that a specific test probe can be designed for a custom testing process. Patients who do not have a detailed genetic testing report are usually asked to come to Cyprus twice- one for leaving a blood sample in order for a thorough mutation testing to be performed, after which a test probe can be custom-bıilt, and a second time for the IVF process.
Success and Limitations:
PGT-M provides nearly 98–99% accuracy in preventing the transmission of genetic conditions when performed in accredited laboratories (Kuliev et al., 2020). However, challenges include the need for detailed genetic workup of the couple and the possibility of insufficient embryos for testing. Women in older age brackets with diminished ovarian reserves can sometimes benefit from multiple rounds of egg collection in order to maximize the number of embryos that will be obtained. In such cases, an egg retrieval will be scheduled during both trips.
3. PGT-SR (Preimplantation Genetic Testing for Structural Rearrangements)
PGT-SR is aimed at detecting chromosomal structural abnormalities, such as translocations, inversions, or duplications. Such rearrangements can lead to unbalanced embryos, causing miscarriage or congenital abnormalities. Patients with balanced translocations often do not show any symptoms themselves. However, when they are trying for a pregnancy, some of the resulting embryos have deadly chromosomal aberrations, resulting in failed pregnancies or recurrent miscarriages. Individuals with balanced chromosomal rearrangements, such as Robertsonian or reciprocal translocations, often undergo PGT-SR to ensure the selection of balanced embryos that will not lead to miscarriage or developmental disorders (Munné et al., 2020).
Indications:
Carriers of balanced chromosomal translocations (e.g., Robertsonian or reciprocal)
Couples with a history of recurrent miscarriage or offspring with structural chromosomal abnormalities.
Procedure:
PGT-SR employs methods like NGS to detect structural abnormalities, essentially using a similar testing procedure to PGT-A.
Success and Limitations:
PGT-SR significantly reduces the risk of miscarriage in translocation carriers, with studies reporting clinical pregnancy rates of 50–70% compared to lower rates in untreated cycles (Collins et al., 2021). However, this approach may not completely eliminate the risk of abnormal outcomes, as testing only evaluates chromosomal structure and not gene function. If there are additional genetic issues, this test will not address them. Nevertheless, this would have a very low incidence.
Efficacy and Clinical Impact of PGT
Implantation Rates and Live Birth Rates
PGT, particularly PGT-A, has shown promise in improving implantation rates and live birth rates in specific populations, such as women over 35 or those with recurrent implantation failure. For PGT-M and PGT-SR, the primary success measure is the prevention of genetic or chromosomal conditions in offspring, with high accuracy rates reported in numerous studies (Practice Committee of the ASRM, 2020).
Reduction in Miscarriage Rates
PGT-A has been linked to lower miscarriage rates, especially in patients with recurrent pregnancy loss. The detection and exclusion of aneuploid embryos significantly reduce pregnancy loss in these cases. Couples with a history of recurrent miscarriages, especially due to chromosomal abnormalities, benefit from PGT to improve the likelihood of a successful pregnancy by selecting chromosomally normal embryos (Carp, 2018).
Male Factor Infertility: Severe male infertility cases may increase the risk of chromosomal abnormalities in embryos, making PGT-A advisable in such cases to reduce this risk (Kushnir et al., 2016).
Procedure of Pre-implantation Genetic Testing
PGT can only be offered as part of an IVF (In vitro fertilization) cycle because this is the only way that embryos can be created in a lab environment in order to undergo biopsy and testing procedures. The PGT process involves several key steps within an IVF cycle:
1. Ovarian Stimulation and Egg Retrieval: First, the woman undergoes ovarian stimulation with hormonal medications to produce multiple eggs. These eggs are then retrieved from the ovaries via a minor surgical procedure called ‘oocyte pick up’ (Practice Committee of the American Society for Reproductive Medicine, 2018). Women with highly diminished ovarian function may be required to undergo multiple egg retrievals in order to obtain a sufficient number of embryos to be tested. Keep in mind that higher the number of embryos, higher the likelihood of obtaining viable embryos for transfer.
2. Fertilization and Embryo Culture: The retrieved eggs are fertilized in the laboratory with sperm, typically using intracytoplasmic sperm injection (ICSI) to ensure only one sperm enters each egg. This process minimizes the risk of contamination from additional sperm cells, which could otherwise affect the genetic testing results (Scott et al., 2013).
3. Embryo Biopsy: On day five after fertilization, embryos reach the blastocyst stage. At this point, a few cells are carefully removed from the embryo’s outer layer (trophectoderm) for genetic testing. This biopsy procedure does not appear to harm the embryo’s development or implantation potential as only a few cells are extracted (Benoff et al., 1999).
4. Genetic Analysis: The biopsied cells undergo genetic analysis using techniques like next-generation sequencing (NGS), fluorescent in situ hybridization (FISH), or polymerase chain reaction (PCR). NGS has become the preferred method for PGT-A due to its high accuracy in detecting chromosomal abnormalities (Franasiak et al., 2014).
5. Embryo Transfer: Once the genetic testing results are available, embryos identified as free from the targeted genetic abnormalities or chromosomal issues are selected for transfer into the woman’s uterus. Testing often takes a few days. This means that the embryos are usually not transferred within the same cycle as the IVF procedure. Normally, day 5 blastocyst formation stage is when the embryo transfer takes place (approximately day 20 of the woman’s menstrual cycle). When genetic testing takes a few days, this embryo transfer window is missed, meaning, the patient will need to be prepared for an embryo transfer in the next menstrual cycle. This is done by freezing embryos after the biopsy process.
Preimplantation genetic testing is a transformative tool in reproductive medicine, enabling improved outcomes in IVF cycles and the prevention of genetic diseases. Each type of PGT—PGT-A, PGT-M, and PGT-SR—has distinct indications and benefits, making it essential to tailor its use to individual patient circumstances.
For more information on our PGT protocols and IVF procedured, use our contact form to contact us.
References
Benoff, S., Hurley, I. R., Cooper, G. W., Mandel, F. S., Rosenfeld, D. L., & Hershlag, A. (1999). Numerical dose-compensated in vitro fertilization inseminations yield high fertilization and pregnancy rates. Fertility and Sterility, 71(6), 1067–1072. https://doi.org/10.1016/s0015-0282(99)00311-8.
Carp, H. (2018). “Recurrent Pregnancy Loss: Causes, Controversies, and Treatment.” Best Practice & Research Clinical Obstetrics & Gynaecology, 53, 3-12. doi:10.1016/j.bpobgyn.2018.08.005.
Collins, S. C., Zegers-Hochschild, F., & Cobo, A. (2021). Preimplantation genetic testing for structural rearrangements: Success rates and challenges. Fertility and Sterility, 115(5), 1201–1210.
Fragouli, E., Alfarawati, S., Spath, K., & Wells, D. (2017). “The Origin and Impact of Embryo Aneuploidy in Human IVF Practice.” Cytogenetic and Genome Research, 150(3-4), 217-227. doi:10.1159/000478888.
Franasiak, J. M., et al. (2014). “Next Generation Sequencing for Pre-implantation Genetic Screening of Aneuploidy as an Alternative to Array Comparative Genomic Hybridization.” Molecular Cytogenetics, 7, 19. doi:10.1186/1755-8166-7-19.
Frankel, M. S., & Chapman, A. R. (2018). “Ethical and Policy Issues in Genetic Testing and Screening of Children.” Genetics in Medicine, 20(4), 435-441. doi:10.1038/gim.2017.210.
Geraedts, J., & Sermon, K. (2016). “Pre-implantation Genetic Testing: Recent Developments and Future Prospects.” Human Reproduction Update, 22(4), 402-405. doi:10.1093/humupd/dmw007.
Greco, E., et al. (2015). “Double Cleavage of the Zygote: A Novel Indicator of Embryo Development.” Fertility and Sterility, 103(6), 1290-1296. doi:10.1016/j.fertnstert.2015.02.025.
Kuliev, A., Rechitsky, S., & Tur-Kaspa, I. (2020). Preimplantation genetic testing for monogenic disorders: Twenty-five years of experience. Reproductive Biomedicine Online, 41(3), 379–390.
Kushnir, V. A., Solouki, S., Darmon, S. K., Barad, D. H., & Gleicher, N. (2016). Systemic inflammation and autoimmunity in women with chronic endometritis. American Journal of Reproductive Immunology, 75(6), 672–677. https://doi.org/10.1111/aji.12508
Munné, S., Spinella, F., & Grifo, J. A. (2019). Clinical outcomes after the application of PGT-A in IVF cycles: A review. Human Reproduction Update, 25(2), 209–222.
Practice Committee of the American Society for Reproductive Medicine (ASRM). (2020). Clinical applications of preimplantation genetic testing: A committee opinion. Fertility and Sterility, 113(2), 305–322.
Scott, R. T., Jr, Upham, K. M., Forman, E. J., Zhao, T., & Treff, N. R. (2013). Cleavage-stage biopsy significantly impairs human embryonic implantation potential while blastocyst biopsy does not: A randomized and paired clinical trial. Fertility and Sterility, 100(3), 624–630. https://doi.org/10.1016/j.fertnstert.2013.04.039
North Cyprus IVF Centre
North Cyprus IVF Centre is a patient focused fertility clinic, located within “Elite Research and Surgical Hospital” in Nicosia, Cyprus. Our clinic is one of the most advanced fertility clinics in the world, offering a wider selection of treatment options at affordable prices.
Contact Us
Phone
English: +90 548 875 8000
French: +90 548 876 8000
Turkish: +90 542 869 8000
Arabic: +90 548 875 8000
German: +90 548 830 1987
Russian: +90 548 828 9955
info@northcyprusivf.net
© 2020 LowCostIVF - All rights reserved. Privacy Policy