- About
- Blog
- Infertility
- IVF Treatments
- New IVF Advances
- Mitochondrial Replacement Therapy!
- IVF Treatment in Cyprus
- IUI
- Mini IVF
- IVF + ICSI
- Cytoplasmic IVF
- Tandem IVF Cycle
- Egg Donation
- Embryo Donation
- Sperm Donation
- Gender – Sex Selection
- Gestational Surrogacy
- Same Sex Gay Surrogacy
- Surgical Sperm Retrieval
- Pre Implantation Genetic Diagnosis PGD
- Egg Freezing
- Gender Selection Using Donor Eggs
- Sickle Cell Disease Prevention
- F.A.Q.
- Travel
- About
- Blog
- Infertility
- IVF Treatments
- New IVF Advances
- Mitochondrial Replacement Therapy!
- IVF Treatment in Cyprus
- IUI
- Mini IVF
- IVF + ICSI
- Cytoplasmic IVF
- Tandem IVF Cycle
- Egg Donation
- Embryo Donation
- Sperm Donation
- Gender – Sex Selection
- Gestational Surrogacy
- Same Sex Gay Surrogacy
- Surgical Sperm Retrieval
- Pre Implantation Genetic Diagnosis PGD
- Egg Freezing
- Gender Selection Using Donor Eggs
- Sickle Cell Disease Prevention
- F.A.Q.
- Travel
IVF Success Rates at North Cyprus IVF Center
Why does North Cyprus IVF Centre has such high success rates
IVF Treatment Success – What Are the Factors Behind Success in an IVF Cycle?
In vitro fertilization (IVF) success is influenced by a complex interplay of various factors ranging from medical conditions and lifestyle choices to the technical aspects of the IVF procedure itself. Understanding these factors can help patients and clinicians optimize the chances of a successful outcome. At North Cyprus IVF Center, we understand that success of an IVF cycle is what makes a difference in a couple’s life. Let’s take a look at factors determining the success of an IVF treatment.
1. Age of the Female Patient
Age is the single most important factor in IVF success. However, this is not an attribute to age as a number, but more so for what it represents from a reproductive point of view. The age of a woman is critically important in IVF success primarily due to its impact on egg quality and quantity, which are decisive factors in the outcomes of IVF treatments. Following are some of the biological and physiological mechanisms that link a woman’s age to IVF success rates:
- 1a. Ovarian Reserve Decline
Ovarian reserve refers to the pool of eggs present in the ovaries at any given time. Women are born with a finite number of oocytes, and this number progressively declines with age. Techniques such as Anti-Müllerian Hormone (AMH) testing and antral follicle counts (AFC) through ultrasound are used to evaluate ovarian reserve. Both AMH levels and AFC decrease as women age, signaling a reduced ovarian reserve. - 1b. Egg Quality Deterioration
With advancing age, the genetic integrity of oocytes diminishes. This is primarily due to increased incidence of chromosomal abnormalities, such as aneuploidy—the presence of an abnormal number of chromosomes in a cell. Aneuploidy rates in eggs significantly increase as women approach their mid-30s and beyond. There are a few reasons behind this genetic issue. The spindle apparatus, which is crucial for chromosome segregation during cell division, shows impaired function in older eggs. This impairment leads to errors in meiotic divisions, particularly during the division of meiotic spindles, which can result in uneven chromosomal separation and aneuploidy. Beyond chromosome segregation, the aging oocyte also accumulates damage to its cytoplasmic structures, mainly, the mitochondria. Eggs require substantial energy for maturation, fertilization, and early embryonic development. Mitochondria are the primary source of this energy, and their functionality and ability to balance reactive oxygen species (ROS) damage declines with age. Decreased mitochondrial function can lead to insufficient energy for critical cellular processes, affecting oocyte maturation and embryo development post-fertilization. Therefore, chromosomal problems as well as mitochondrial insufficiency bring about what we call “oocyte aging”. There are certain lifestyle modifications and supplements that can be taken in order to optimize mitochondrial age in older brackets. This is explained in detail in our “Oocyte Anti-Aging Protocol” page. - 1c. Hormonal Changes
With advancing age, there is often a decline in the responsiveness of the ovaries to follicle-stimulating hormone (FSH). This decreased responsiveness can result in poorer outcomes in response to the hormonal treatments used in IVF to stimulate the ovaries to produce multiple eggs.
The cumulative effect of these factors explains why the age of a woman is a pivotal determinant of IVF success. It influences both the chances of obtaining viable, genetically normal oocytes and the capability of these oocytes to develop into healthy embryos capable of successful implantation and pregnancy. This complex interplay underscores the challenges faced in reproductive medicine as maternal age increases, highlighting the importance of tailored approaches to IVF that consider the age and specific reproductive health profile of each patient.
2. Sperm Quality
The quality of the sperm used can also affect IVF success. Factors such as sperm motility (the ability of sperm to move efficiently), morphology (the shape and size of sperm), and concentration are crucial. Poor sperm quality can lead to issues with fertilization and embryo development.
Sperm quality is crucial in determining the success of in vitro fertilization (IVF) due to its fundamental role in the fertilization process and subsequent embryo development. Sperm quality is typically assessed by parameters such as concentration, motility, morphology, and DNA integrity. Below are the main considerations when talking about sperm quality:
- 2a. Sperm Concentration
Sperm concentration, or count, refers to the number of spermatozoa per unit of semen. A higher sperm count increases the probability of successful egg fertilization because more sperm are available to attempt entry into the egg. Lower sperm counts can be indicative of hypogonadism or other hormonal imbalances, which might affect other sperm parameters like motility and morphology. When sperm concentration is low, so is the likelihood of natural conception as not enough sperm cells will be able to complete the journey into the fallopian tubes in the female reproductive tract. In such cases, ICSI during an IVF cycle can provide additional benefits. - 2b. Sperm Motility
Sperm motility describes the ability of sperm to move efficiently through the female reproductive tract or through culture medium in IVF. Effective motility is essential for reaching and penetrating the egg. Motility is powered by ATP generated by mitochondria located in the sperm’s midpiece. The integrity and functionality of these mitochondria are crucial; any mitochondrial DNA mutations can reduce ATP production, thereby impairing motility. Similarly, mitochondrial aging can be a contributing factor in impaired motility. - 2c. Sperm Morphology
Morphology refers to the size, shape, and structure of sperm. Normal morphology is a predictor of a sperm’s ability to fertilize an egg, as it affects the sperm’s ability to swim to and penetrate the egg. Structural anomalies in the sperm head can affect the acrosome reaction—a critical release of enzymes that allows the sperm to penetrate the outer layers of the egg. Furthermore, structurally abnormal sperm shape can also be an indication of a more serious underlying issue, such as the genetic integrity of the sperm.
The integrity of sperm DNA is vital. DNA fragmentation in sperm can result from oxidative stress or apoptosis during spermatogenesis. High levels of DNA fragmentation are associated with reduced fertilization rates, poor embryo development, and lower pregnancy rates. Oxidative stress leads to the production of reactive oxygen species (ROS) which can damage the DNA in sperm. Antioxidant defense mechanisms are crucial in protecting sperm DNA from oxidative damage. More information on improving sperm parameters can be found on our “Sperm Anti-Aging Protocol” page.
Each of these sperm parameters plays a fundamental role in the complex process of fertilization and early embryonic development. The biochemical and physiological health of sperm directly impacts the efficiency of these processes in IVF, influencing outcomes from fertilization success to implantation and beyond. Optimizing sperm health is thus integral to enhancing IVF success rates, underscoring the importance of assessing and addressing any deficiencies in these parameters during fertility treatments. For more information on how to optimize sperm health, you can visit our ‘Sperm Anti-Aging Protocol’ page.
3. Underlying Fertility Issues
The specific reasons for infertility — such as endometriosis, polycystic ovary syndrome (PCOS), uterine abnormalities, or genetic anomalies— can affect the success rates of IVF. Each condition may require specialized approaches during the IVF process.
4. Lifestyle Factors
Lifestyle factors such as smoking, alcohol consumption, excessive weight, and stress are known to affect fertility. Lifestyle cannot be thought of independently from the oocyte and sperm quality issues as lifestyle choices are directly related to these parameters. For instance, oocyte aging is not only a result of internal mechanisms, but also an outcome of what kinds of toxins, chemicals and inflammatory factors a person has been exposed to. Maintaining a healthy weight through diet and exercise, reducing stress, and avoiding tobacco and excessive alcohol can improve the chances of IVF success.
5. Protocol and Medication
It goes without saying that the protocols used for ovarian stimulation need be tailored to a woman’s specific age, hormonal profile, and response in previous cycles. The type and dosage of fertility drugs can affect the number and quality of eggs retrieved.
6. Embryo Quality
Embryo quality can be seen as a combination of egg and sperm quality parameters. However, in a given IVF cycle, not all the embryos will have a correct genetic composition. Even when the patients are quite young, there will still be a small percentage of chromosomal aneuploidy with some embryos. As a female patient’s age goes up, so will the rate of aneuploidy observed in embryos created in an IVF cycle. Techniques like preimplantation genetic testing (PGT) can help select embryos with the highest potential for successful pregnancy. You can read more about embryo quality and grading on our ‘Embryo Grading System‘ page.
7. Laboratory Environment and the Transfer Technique
The quality of the laboratory where the embryos are cultured plays a critical role. Factors such as air quality, temperature, and the expertise of the embryologists can all impact the viability of the embryos. Conditions under which embryos are handled prior to transfer are vital. Factors like temperature, pH, and exposure to light and air can affect embryo viability. Minimizing the time embryos spend outside the incubator and ensuring rapid and careful loading into the catheter are crucial to maintaining their viability.
Similarly, the technique of embryo transfer in IVF is a critical step that significantly affects the success rates of implantation and ongoing pregnancy. The procedure should be as gentle and precise as possible to increase the chances of implantation. This procedure involves transferring embryos into the uterus and is the culmination of the complex IVF process. It appears straightforward, but the subtleties of how the transfer is performed can have profound impacts on the outcome.
The type and flexibility of the transfer catheter can affect the ease and precision of the transfer. Soft catheters are generally preferred as they are less likely to cause trauma to the uterine lining. Trauma and bleeding during an embryo transfer process are known to have a detrimental effect on success outcomes. The skill and experience of the clinician performing the transfer are also paramount. A gentle technique that avoids touching the uterine fundus is crucial to minimize contractions and disruptions that might expel the embryo.
Using ultrasound to guide the embryo transfer enhances precision in depositing the embryo at an optimal location within the uterus, generally 1-2 cm from the uterine fundus.
8. Endometrial Receptivity
The condition of the uterine lining, or endometrium, when the embryo is transferred is key. Adequate preparation of the endometrium, typically using estrogen and progesterone, is essential to make it receptive to the embryo. The thickness and pattern of the endometrial lining, assessed by ultrasound, are indicators of its receptivity. The endometrium has a limited window of receptivity, known as the implantation window. Misalignment between the embryo’s developmental stage and this window can reduce the likelihood of successful implantation. This synchronization between the development stage of the embryo (whether it’s a day-3 or a blastocyst on day-5) and the phase of the endometrial cycle is key.
9. Psychological Factors
The psychological stress associated with undergoing IVF can impact its success. Ensuring that the patient is relaxed and comfortable during the procedure can reduce uterine contractions, which might affect embryo placement. Psychological support and counseling as well as relaxation and mindfulness techniques prior to the embryo transfer procedure might help alleviate stress and improve outcomes.
Successful IVF depends on carefully balancing and optimizing all of these factors. For prospective parents, understanding these elements can help in making informed decisions about their treatment options.
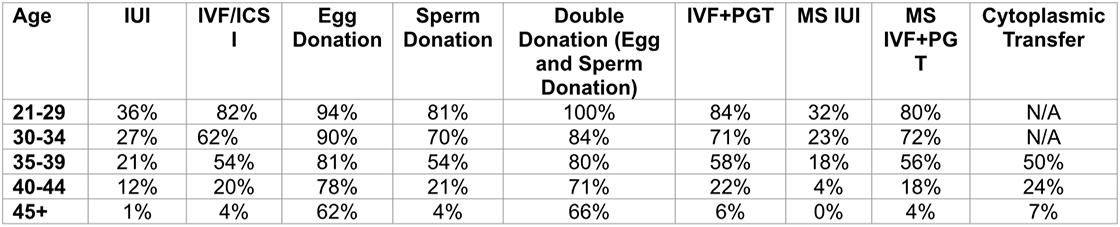
IVF Success Rates at North Cyprus IVF Center for the year 2023:
Why does North Cyprus IVF Centre has such high success rates?
North Cyprus IVF Centre is a patient-centered fertility clinic which not only treats, but also researches and produces clinical studies. With an active quest for knowledge and improvement, our clinic is one of the most advanced fertility clinics in the world. There are several factors that contribute to the success of North Cyprus IVF Centre. These include:
Accumulation of know-how and experience within the past 24 years as we are the very first fertility treatment clinic in the region. Practice makes perfect! As the oldest clinic in Northern Cyprus, we reserve the first place to ourselves when it comes to successful IVF outcomes! In a 24 year-old IVF clinic, there are no rooms for trial and error.
We are not just an IVF clinic, but also a research centre with own research team who investigate the underlying causes of infertility both at the patient level and the global level, allowing us to provide you with customized care. Our genetics laboratory and our clinical trial programs provide us constant support for improving our approaches and excelling at what we do.
Our egg donor program only admits donors aged between 19-25 who have donated before and contributed to a positive pregnancy, therefore, we only use pregnancy proven fertile and healthy egg donors which is one of the main contributors of success in donor program. This is precisely why we have been named the “Leading IVF Clinic in Donor Egg treatments”. Success rates for IVF with egg donation tends to run higher than 70% as an overall rate at North Cyprus IVF Clinic.
We are able to transfer up to 3 embryos legally, increasing your chances of success with IVF treatments compared to a lower number of embryos transferred. It is not just the number of embryos that matters, but the quality of these embryos as well that make all the difference when it comes to success. Our MicroChip sperm selection method and our time-lapse embryo screening systems allow us to make sure we offer you a state of the art treatment which aims to maximize the quality of your embryos during your IVF cycle.
We offer ICSI (Intra-Cytoplasmic Sperm Injection) free of charge as a standard procedure with all our IVF treatments to all our patients.
We are able to offer non-conventional methods and approaches such as Cytoplasmic Transfer, MRT, Ovarian PRP to patients in older age brackets as well as many other clinical trials to patients who qualify. This is also a factor which contributes to success via improved embryo quality.
We make sure that you are offered a custom prepared treatment protocol geared toward your specific needs and requirements.
And finally, Dr. Savas is a pioneer in the field of infertility!
Topics related to North Cyprus IVF Center
North Cyprus IVF Centre
North Cyprus IVF Centre is a patient focused fertility clinic, located within “Elite Research and Surgical Hospital” in Nicosia, Cyprus. Our clinic is one of the most advanced fertility clinics in the world, offering a wider selection of treatment options at affordable prices.
Contact Us
Phone
English: +90 548 875 8000
French: +90 548 876 8000
Turkish: +90 542 869 8000
Arabic: +90 548 875 8000
German: +90 548 830 1987
Russian: +90 548 828 9955
info@northcyprusivf.net
© 2020 LowCostIVF - All rights reserved. Privacy Policy

